Nutritional assessment of under five children in a rural belt of southern Rajasthan, India
Kumar L. D.1, Mangal N.2*, Varghese K A.3, Chand Salvi T.4, Prakash Salvi P.5, Singh Udawat V.6
DOI: https://doi.org/10.17511/ijphr.2019.i6.03
1 Dilip Kumar L., Associate Professor, Department of Community Medicine, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
2* Nitesh Mangal, Assistant Professor, Department of Community Medicine, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
3 Varghese K A, Statistician, Department of Community Medicine, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
4 Tara Chand Salvi, Medical Social Worker, Department of Community Medicine, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
5 Prem Prakash Salvi, Medical Social Worker, Department of Community Medicine, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
6 Vijaypal Singh Udawat, Health Inspector, Department of Community Medicine, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India.
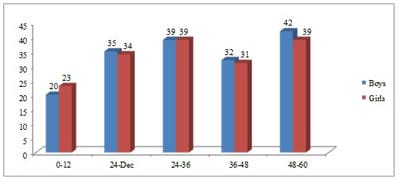
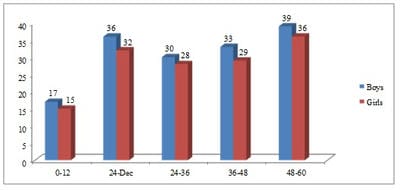
Introduction: Despite the importance given by WHO and its member countries, malnutrition of children continued to be a serious problem world-wide, especially in developing countries like India. The uneven magnitude of this problem across Indian states reveals the need for ascertaining the magnitude of malnutrition. Aims & Objectives: The present study is aimed to ascertain the magnitude and the factors affecting the malnutrition across tribal and non-tribal communities in a rural belt of southern Rajasthan. Materials & Methods: The cross-sectional study carried out during March 2018 to February 2019 covering 200 households each from the two communities included 334 and 295 under five children respectively. Results: The magnitude of moderately and severely underweight children was 32.63% and 7.49% in tribal and 24.41% and 4.41% in non-tribal communities. With respect to stunting and Body Mass Index, 64.37% and 63.47% in tribal and 73.22% and 73.90% in non-tribal were found normal. The factors like household income and mother’s literacy were found strongly associated with malnutrition. Conclusion: Nutrition, health education and good access, and utilization of healthcare with separate strategic intervention for tribal and non-tribal children can be very effective interventions to overcome the burden of malnutrition.
Keywords: Malnutrition, Underweight, Stunting, Under-five children, Body Mass Index
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Community Medicine, Pacific Institute of Medical Sciences, Udaipur, Rajasthan, India. Email: |
Kumar LD, Mangal N, Varghese K A, Salvi TC, Salvi PP, Udawat VS. Nutritional assessment of under five children in a rural belt of southern Rajasthan, India. Public Health Rev Int J Public Health Res. 2020;6(6):224-233. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/125 |


 ©
©