Self medication pattern and awareness about antibiotic resistance in urban area of Pune
S Mhaske M.1*, S khismatrao D.2, D Gore H.3, Sable S.4
DOI: https://doi.org/10.17511/ijphr.2015.i4.03
1* Mayavati S Mhaske, Department of community Medicine, Smt. Kashibai navale medical college, Pune, Maharashtra, India.
2 Deepak S khismatrao, Ex Associate professor, Department of community Medicine, Smt. Kashibai navale medical college, Pune, Maharashtra, India.
3 Harishchandra D Gore, Department of community Medicine, Smt. Kashibai navale medical college, Pune, Maharashtra, India.
4 Surekha Sable, Department of community Medicine, Smt. Kashibai navale medical college, Pune, Maharashtra, India.
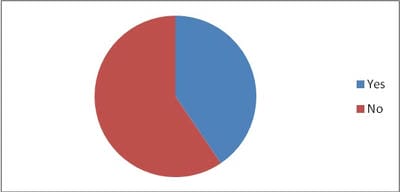
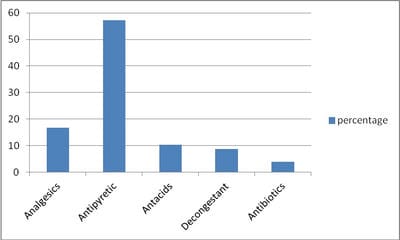
Introduction: self medication is defined as the consumption of medicinal products with the purpose of treating diseases or symptoms, or even promoting health, without the prescription provided by medical professional. Inappropriate self medication results in irrational use of drugs, wastage of resources, increase resistance of pathogens and health hazards and if action is not taken the danger of drug interaction and drug resistance will increase. Methods and Material: This is a cross –sectional study done at outpatient department of urban health training centre. Total 126 adults were interviewed with the help of predesigned Semistructred questionnaire in local language. Statistical analysis used: Data was filled in Excel sheet and proportions were calculated. Results: 51 (40.47%) participants admitted that they were storing some medicine at home. 67(53.17%) participants answered that they are purchasing the medicines without consulting a doctor. 23(18.25%) out of 126 were knowing antibiotics and very few I .e only 5 (3.96%) were aware of the antibiotic resistance. Conclusions: Though the self medication among adults in urban area is high (53.17%) awareness about antibiotic resistance is very low (3.96%).
Keywords: Self Medication, Awareness, Antibiotic Resistance
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Department of community Medicine, Smt. Kashibai navale medical college, Pune, Maharashtra, India. Email: |
Mhaske MS, khismatrao DS, Gore HD, Sable S. Self medication pattern and awareness about antibiotic resistance in urban area of Pune. Public Health Rev Int J Public Health Res. 2015;2(4):38-42. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/17 |


 ©
©