Prevalence of depression and its risk factors among a rural geriatric population of North Kerala
Rose Jacob S.1*, Rapheal L.2, Bina T.3
DOI: https://doi.org/10.17511/ijphr.2015.i4.05
1* Sabitha Rose Jacob, Assistant Professor, Department of Community Medicine, Government Medical College, Manjeri, Kerala, India.
2 Lucy Rapheal, Professor, Department of Community Medicine, Government Medical college, Manjeri, Kerala, India.
3 Thomas Bina, Professor, Department of Community Medicine, Government Medical college, Manjeri, Kerala, India.
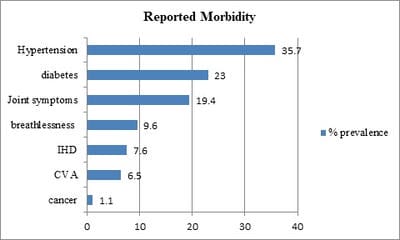
Introduction: Depression in elderly is a common and important health problem causing considerable morbidity and disability. But it is often undetected and neglected as a normal part of aging. Methods: In order to studythe prevalence of depression and its risk factors among rural elderly population a cross sectional study was conducted in the field practice area of Community Medicine department of a tertiary care center of North Kerala. The study population was selected by cluster sampling technique. Data on socio demographic characteristics and morbidity were collected using personal interview schedule. Psychological morbidity was assessed using Geriatric Depression Scale (GDS 15) and elderly cognitive assessment questionnaire(ECAQ). Results: Among a study population of 395, a total of 230(58.2%) had some depression. Females and those with a poor perception of health had higher prevalence. Presence of a chronic morbidity OR=1.3 95%CI (1.02-1.68),cognitive impairment OR=1.2,95%CI(1.02-1.42),physical disability, unmarried statusOR-1.01,95%CI(.85-1.38), being illiterate OR=1.29 95 % CI (1.09-1.52)and staying alone OR=1.3 95% CI (0.96-1.75)were the risk factors found to be significantly associated with depression. Conclusions: Prevalence of depression is high among rural geriatric population and it is associated with risk factors like chronic morbidity, physical disability and low socio economic status which can be managed by timely interventions. Appropriate social and health measures are needed to improve the quality of life of elderly.
Keywords: Depression, Elderly, Risk Factors
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Community Medicine, Government Medical College, Manjeri, Kerala, India. Email: |
Jacob SR, Rapheal L, Bina T. Prevalence of depression and its risk factors among a rural geriatric population of North Kerala. Public Health Rev Int J Public Health Res. 2015;2(4):49-55. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/19 |


 ©
©