Nutritional status and immunization coverage of the Anganwadi children in the Urban Training Health Centre of Travancore Medical College, Kollam
Datta S.1*, Jobby A.2
DOI: https://doi.org/10.17511/ijphr.2016.i1.06
1* Sumit Datta, Associate Professor, Department of Community Medicine, Travancore Medical College, Kollam, Kerala, India.
2 Abraham Jobby, Professor, Department of Forensic Medicine, Travancore Medical College, Kollam, Kerala, India.
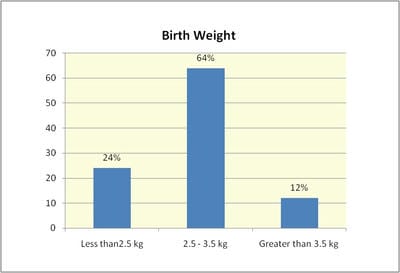
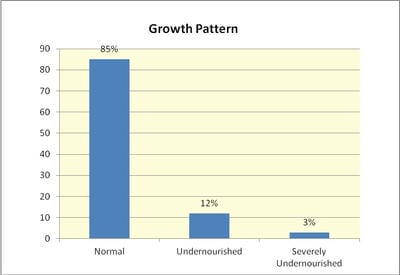
Introduction: Adequate nutrition is an indispensable component of healthy life and access to healthy diet and optimum nutrition are key components of physical, mental and social development for a child. Objective: To assess the Nutritional status among the anganwadi children in the Urban Training Health Centre and to observe the details of the immunization coverage among the same population. Materials and Methods: The present cross sectional study was conducted in seven anganwadi centers, which are selected by convenient sampling. Nutritional status and immunization status was assessed among all the children by a pretested structured questionnaire and analyzed by applying SPSS. Results: Undernourished children in the Anganwadis under study were 15%. DPT booster (16-24months) and DT Booster (5-6 years) were 75% and 3% respectively. Conclusion: We recommend that the low coverage of DPT booster must be immediately corrected in a situation where diphtheria outbreaks are reported from different parts of Kerala.
Keywords: Nutritional Status, Immunization Coverage, Anganwadi
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Community Medicine, Travancore Medical College, Kollam, Kerala, India. |
Datta S, Jobby A. Nutritional status and immunization coverage of the Anganwadi children in the Urban Training Health Centre of Travancore Medical College, Kollam. Public Health Rev Int J Public Health Res. 2016;3(1):27-31. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/23 |


 ©
©