Prevalence of exposure to passive smoking and awareness about its ill effects among medical college undergraduate students in Mangalore
Vinayak J K.1*, Kiran K G.2, Patil S.3, M Shetty S.4, Kiran N U.5, Chethan T K.6
DOI: https://doi.org/10.17511/ijphr.2016.i1.07
1* Vinayak J K, Post graduate, 2 Kiran K G, Professor, 3 Sandeep Patil, Assistant Professor, 4 Shruthi M Shetty, Post Graduate, 5 Udaya Kiran N, Professor and Head; all author are affiliated with Department of Community Medicine, Adhichunchanagiri institute of medical sciences, BG nagar, Mandya, India, 6 Chethan T K, Assistant Professor, Department of Community Medicine Adhichunchanagiri institute of medical sciences, BG nagar, Mandya, India
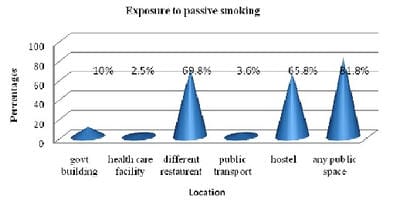
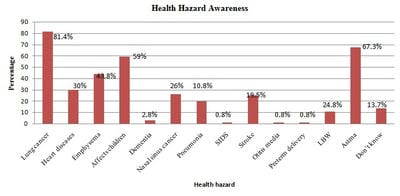
Introduction: Passive smoking, it is the combination of side stream smoke given off by a burning tobacco product and mainstream smoke exhaled by a smoker. Exposure to passive smoking can take place in the home, the workplace or other environment that are accessible to the public places. Aim: To estimate the prevalence of exposure to passive smoking and awareness about its ill effects among Medical colliege undergraduate students in Mangalore. Materials and Method: This was a cross sectional study was conducted among 400 randomly selected undergraduate students in one of the medical college in Mangalore. Data was obtained by using a pre tested, structured questionnaire. Results: Among the total 400 students, 216 were males and 184 were females. Of the 400 students 10.25% were smokers ( 18.9% males, 0% females) 12.75% past smookers (20.3% males, 3.8% females) , 77.0% were non smokers. Awareness of passive smoking among all participants was 86.5% . Most of the people were exposed to passive smoking (96.25%) in public places in last thirty days. 61.5% students were exposed to passive smoking in their hostel daily (males=88.8%, females= 29.3%) . Conclusion: Self-reported tobacco use status, parents tobacco use, close friends smoking, and participants residence were the signaficant determinants of exposure to pasive smoking at home and outside the home.
Keywords: Passive smoking, Undergaduates, Past smoker, Knowledge
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Post graduate, Department of Community Medicine, K. S. Hegde Medical Academy, Nitte University, Mangalore, Karnataka, India. Email: |
Vinayak J K, Kiran K G, Patil S, Shetty SM, Kiran NU, Chethan T K. Prevalence of exposure to passive smoking and awareness about its ill effects among medical college undergraduate students in Mangalore. Public Health Rev Int J Public Health Res. 2016;3(1):32-37. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/27 |


 ©
©