A prospective study on the clinical profile and outcome of patients with hyponatremia in a tertiary care centre in Kerala, South India
Grace N C M.1*, Jacob K J.2, Rajesh K R.3, Vijayan S.4, Jayakrishnan C.5, Fatima6, Mathini S.7
DOI: https://doi.org/10.17511/ijphr.2016.i2.05
1* Mary Grace N C, Associate Professor, Department of Medicine, Government Medical College, Thrissur, Kerala, India.
2 Jacob K J, Additional Professor, Government Medical College, Thrissur, Kerala, India.
3 Rajesh K R, Assistant Professor, Government Medical College, Thrissur, Kerala, India.
4 Sarang Vijayan, Senior Resident, Department of Medicine, Government Medical College, Thrissur, Kerala, India.
5 Jayakrishnan C, Junior Resident, Department of Medicine, Government Medical College, Thrissur, Kerala, India.
6 Fatima, Junior Resident, Department of Community Medicine, Government Medical College, Thrissur, Kerala, India.
7 Mathini S, Senior Resident, Department of Medicine, Government Medical College, Thrissur, Kerala, India.
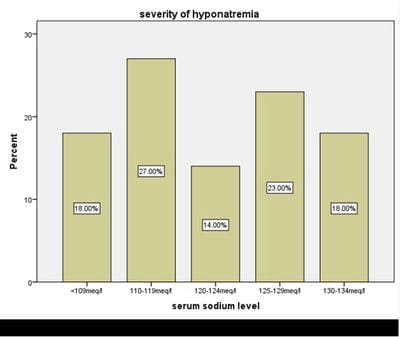
Background: Hyponatremia is the commonest electrolyte disturbance seen in hospitalized patients. The presence of hyponatremia worsens the prognosis in ill patients. Aims: To study the clinical profile and outcome of patients having hypoosmolal hyponatremia. Methods: We studied a total of 100 consecutive patients, with serum sodium concentration less than135meq/l. The study was conducted in a tertiary care centre in Kerala, South India. Those patients with hyponatremia who had normal or high serum osmolality were excluded from the study. Results: There were 55 (55%) male patients and 45 (44%) female patients. The ages ranged from 18 years to 88 years, with a mean age of 60+/-16 years. The most common precipitating factor was neurological and lung conditions. Majority of the patients were asymptomatic at the time of detecting hyponatremia. Majority of the patients were euvolemic at the time of detection of hyponatremia. Conclusion: The conclusion we have drawn from this study is that euvolemic hyponatremia with urine sodium wasting is a more common cause for hyponatremia than conditions leading to hypovolemia. Since majority of the cases are asymptomatic, estimation of the serum electrolytes should be done as a routine in all hospitalized patients. Early recognition of hyponatremia and appropriate intervention would go a long way in improving the outcome.
Keywords: Hyponatremia, Euvolemic hyponatremia, Syndrome of inappropriate antidiuresis, Free water clearance
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Medicine, Government Medical College, Thrissur, Kerala, India. Email: |
Mary Grace N C, Jacob K J, Rajesh K R, Vijayan S, Jayakrishnan C, Fatima, Mathini S. A prospective study on the clinical profile and outcome of patients with hyponatremia in a tertiary care centre in Kerala, South India. Public Health Rev Int J Public Health Res. 2016;3(2):70-74. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/34 |


 ©
©