Prevalence of dropout in measles immunization coverage among children in Kanyakumari District, Tamilnadu
M. Mathiarasu A.1, Anantha Raman V. V.2*, M. Mathew A.3
DOI: https://doi.org/10.17511/ijphr.2017.i1.05
1 Alber M. Mathiarasu, Assistant Professor, Kanyakumari Government Medical College, Asaripallam, Tamil Nadu, India.
2* Anantha Raman V. V., MD, Associate Professor, Department of Community Medicine, SRM Medical College and Research Centre, Kanchipuram, Tamil Nadu, India.
3 Arumai M. Mathew, MSW, PGDCHM, Department of Community Medicine, SRM Medical College and Research Centre, Kanchipuram, Tamil Nadu, India.
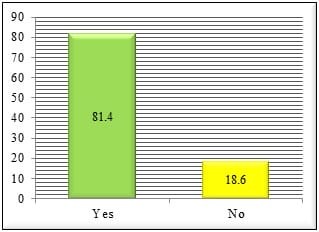
Background: Measles is highly prevalent across globe and it is the main cause for childhood mortality and morbidity. It has now come down in developed countries that worked to prevent transmission. It is still continuing to be a widespread disease in developing countries like India. Objective: To ascertain measles immunization coverage, factors leading to drop-outs and parents’ knowledge, attitude and perceived practices on it. Materials and Methods: A community based cross-sectional study design was adopted to study the children’s dropout in measles immunization. 210 children aged between 12 and 23 months in Kanyakumari district had been picked up from the entire population of 182519 using 30 X 7 cluster random sampling. Results: The study has shed some light on the coverage of measles vaccination of 81.4% with dropout of 18.6%. There were no statistically significant associations between area of residence, place of birth, sex, parental marital status, mothers’ pregnancy status & availability of immunization card and dropouts. In regards to their parents’ knowledge, attitude and perceived practices on Measles, 93.3% had vast awareness. Conclusion: A few factors like ignorance, long gap between administration of two vaccinations, lack of awareness on adverse impact of Measles, have hampered the program from reaching all children in the district. However, these challenges might be addressed through increasing the level of awareness among the parents, identification of dropout cases, scaling up of vaccination programs at gross root level, etc.
Keywords: Dropout, Measles, Mortality, Morbidity, Under-five Children
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , MD, Associate Professor, Department of Community Medicine, SRM Medical College and Research Centre, Kanchipuram, Tamil Nadu, India. Email: |
Mathiarasu AM, Raman VVA, Mathew AM. Prevalence of dropout in measles immunization coverage among children in Kanyakumari District, Tamilnadu. Public Health Rev Int J Public Health Res. 2017;4(1):26-30. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/57 |


 ©
©