Cardiovascular Disease (CVD) Risk estimation among 40 years and older using WHO/ISH risk prediction charts
Singh G.1*, S Nanda G.2, Singh H.3
DOI: https://doi.org/10.17511/ijphr.2017.i5.05
1* Gurpreet Singh, Station Health Organisation, Jalandhar, Punjab, India.
2 Gurprit S Nanda, Professor, Department of Community Medicine, Punjab Institute of Medical Sciences, Jalandhar, Punjab, India.
3 Harinder Singh, Department of Community Medicine, Punjab Institute of Medical Sciences, Jalandhar, Punjab, India.
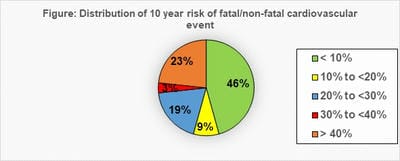
Introduction: Evidence based programme to reduce fatal/non-fatal CVDs can be formulated using WHO/ISH risk prediction charts. Use of combined risk approach is effective in identification of individuals requiring intervention. Objective: To determine 10 year cardiovascular risk and prevalence of selected risk factors for CVDs among 40 years and older population in an urban field practice area of a medical college. Material and methods: This was a cross sectional study conducted with sample size of 116. Inclusion criteria was age >40 years and without CVDs. WHO/ISH risk charts were used. Pilot tested, structured, interview based questionnaire was administered followed by clinical examination to determine prevalence of selected CVD risk factors in the community. Results: Mean age was 56.23 + 10.6 years and majority (74.1%) were females. High 10 year risk of cardiovascular events, family history of CVDs, high BMI, increased risk of metabolic complications, abdominal obesity, hypertension and smoking was seen in 23%, 33.6%, 79.3%, 44.8%, 52.6%, 56.9% and 10.3% respectively. Significant gender difference was seen in prevalence of smoking, physical inactivity, overweight, increased risk of metabolic complications, and abdominal obesity (p= 0.044, 0.036, 0.000, 0.000, and 0.001 respectively). Higher prevalence of Hypertension, Diabetes, abdominal obesity, overweight, and smoking was found in individuals at high 10 year risk of CVD event. Conclusion: The present study document high 10-year risk of cardiovascular events and prevalence of risk factors. Identification of individuals at high risk of CVDs is crucial to mitigate rapidly growing CVD burden in the country.
Keywords: Cardiovascular risk, Body Mass Index, Waist Circumference, Diabetes, Hypertension
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , , , Station Health Organisation, Jalandhar, Punjab, India. Email: |
Singh G, Nanda GS, Singh H. Cardiovascular Disease (CVD) Risk estimation among 40 years and older using WHO/ISH risk prediction charts. Public Health Rev Int J Public Health Res. 2017;4(5):134-140. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/73 |


 ©
©