Acute coronary syndrome in elderly – risk factors and in-hospital outcome
Grace M.1, Chelakkat M.2*, Asokan A.3
DOI: https://doi.org/10.17511/ijphr.2018.i2.05
1 Mary Grace, Associate Professor, Department of Medicine, Medical College Hospital, Thrissur, Kerala, India.
2* Mukundan Chelakkat, Assistant Professor, Department of Cardiology, Medical College Hospital, Thrissur, Kerala, India.
3 Anjana Asokan, Junior Resident, Department of General Medicine, Medical College Hospital, Thrissur, Kerala, India.
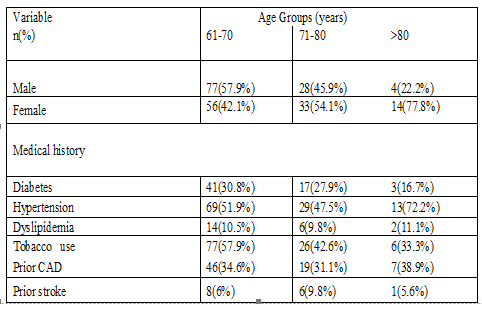
Background: Elderly patients constitute a majority subset of population developing acute coronary syndrome. But specific risk factors and in-hospital outcome have not been well-studied. Objectives: To study the risk factors and in-hospital outcome of people aged >60 years with acute coronary syndrome. Materials and Methods: 220 patients aged >60 years admitted with acute coronary syndrome under Department of General Medicine (during a time period from 1st January 2015 to 31st December 2015) were studied between admission and death/discharge. All patients who opted for primary PCI and who left treatment before completion were excluded. Patients were grouped into STEMI, NSTEMI and unstable angina. Various factors affecting mortality were studied. Results: After exclusion, 212 patients were included in the study. The mean age of men was 68±6 years while that of women was 71±7 years) (p=0.01). Modifiable risk factors were present in 84.9% (n=180), most common risk factor observed was past history of systemic hypertension. (52.36%) (n=111). Hypertension was found to have significant association with mortality. (p value=0.05). Chest pain was the most common symptom. Atypical features were found to be higher in those aged above 80 years. (p value = 0.04). Thrombolysis was not done in 15.7% (16) patients with STEMI, reason being they were out of window period for thrombolysis Women were found to have more pre-hospital delay (p value= 0.026) High Killip class and also hypotension during admission was found to be associated with increased mortality (p value<0.001). Conclusion: Hypertension still remains as an important modifiable risk factor for coronary artery disease in the elderly population. Hence regular monitoring of blood pressure and proper management has to be followed in this age group also. The delay to reach the hospital should be avoided, because thrombolytic therapy is very effective in elderly patients.
Keywords: Acute Coronary Syndrome, Elderly, Risk factors, In- hospital outcome
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Cardiology, Medical College Hospital, Thrissur, Kerala, India. Email: |
Grace M, Chelakkat M, Asokan A. Acute coronary syndrome in elderly – risk factors and in-hospital outcome. Public Health Rev Int J Public Health Res. 2018;5(2):77-81. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/86 |


 ©
©