Prevalence and associated risk factors of depression among housewives in rural Saharanpur, Uttar Pradesh, India
Vikramaditya B.1, Kumar Jha A.2*, Kumar S.3, M.4, Joshi H.5
DOI: https://doi.org/10.17511/ijphr.2020.i1.02
1 Bibhava Vikramaditya, Assistant Professor, Department of Community Medicine, SMMH Government Medical College, Saharanpur, Uttar Pradesh, India.
2* Amit Kumar Jha, Professor, Department of Community Medicine, SMMH Government Medical College, Saharanpur, Uttar Pradesh, India.
3 Sanjeev Kumar, Associate Professor and Head, Department of Community Medicine, SMMH Government Medical College, Saharanpur, Uttar Pradesh, India.
4 Manjeeta , Junior Resident, Department of Community Medicine, SMMH Government Medical College, Saharanpur, Uttar Pradesh, India.
5 Hari Shankar Joshi, Professor and Head, Department of Community and Family Medicine, All India Institute Of Medical Sciences, Gorakhpur, Uttar Pradesh, India.
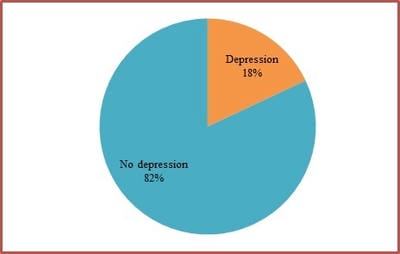
Introduction: Depression is the most common mental disorder. Women and the elderly have shown greater vulnerability to depression. Additional responsibilities due to modernization in rural areas have to lead to increased stress and tension among housewives. Limited data is available on depression among housewives in rural India especially Uttar Pradesh. Objective: To assess the prevalence and risk factors of depression among housewives in the rural area. Methods: The study was done in five villages of Saharanpur, Uttar Pradesh from November 2018 to October 2019. A total of 500 housewives were selected by systematic random sampling. Interviews were conducted by the house to house visits. Depression was evaluated using the self-reported instrument Patient Health Questionnaire-9 (PHQ-9). Results: The prevalence of depression was found to be 18%. There was an increasing trend in the prevalence of depression in the middle age group. The increasing level of education, marriage, better socio-economy, economic independence and absence of co-morbid conditions had a lower prevalence of depression.Conclusion: Housewives should be educated about warning signs and symptoms of depression and motivated to seek professional help.
Keywords: Housewives, Depression, Rural, Saharanpur
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Community Medicine, SMMH Government Medical College, Saharanpur, Uttar Pradesh, India. Email: |
Vikramaditya B, Jha AK, Kumar S, Manjeeta, Joshi HS. Prevalence and associated risk factors of depression among housewives in rural Saharanpur, Uttar Pradesh, India. Public Health Rev Int J Public Health Res. 2020;7(1):7-13. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/132 |


 ©
©