Prevalence and associated risk factors of depression among housewives in rural Saharanpur, Uttar Pradesh, India
Abstract
Introduction: Depression is the most common mental disorder. Women and the elderly have shown greater vulnerability to depression. Additional responsibilities due to modernization in rural areas have to lead to increased stress and tension among housewives. Limited data is available on depression among housewives in rural India especially Uttar Pradesh. So, the present study was planned to assess the prevalence of depression and its associated risk factors among housewives aged 18-59 years in the rural area of district Saharanpur, Uttar Pradesh.
Objective: To assess the prevalence and risk factors of depression among housewives in the rural area.
Methods: The study was done in five villages of Saharanpur, Uttar Pradesh from November 2018 to October 2019. A total of 500 housewives were selected by systematic random sampling. Interviews were conducted by the house to house visits. Depression was evaluated using the self-reported instrument Patient Health Questionnaire-9 (PHQ-9). The analysis was done using MS Excel software and SPSS software version 22.
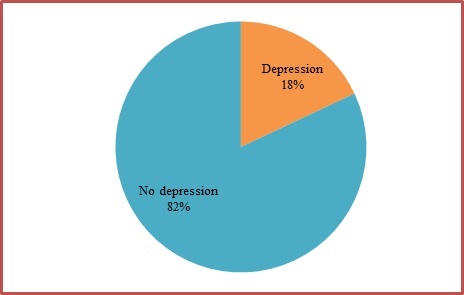
Results: The prevalence of depression was found to be 18%. There was an increasing trend in the prevalence of depression in the middle age group. The increasing level of education, marriage, better socio-economy, economic independence and absence of co-morbid conditions had a lower prevalence of depression. None of the depressed subjects had taken professional help.
Conclusion: Housewives should be educated about warning signs and symptoms of depression and motivated to seek professional help.
Downloads
References
Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575-1586. doi: http://dx.doi.org/10.1016/S0140-6736(13)61611-6.
Math S, Chandrashekar CR, Bhugra D. Psychiatric epidemiology in India. Indian J Med Res. 2007;126(3):183-192.
Ganguli HC. Epidemiological findings on the prevalence of mental disorders in India. Indian J Psychiatry. 2000;42(1):14-20.
World Health Organization. Mental health atlas 2011. Geneva:WHO [Internet] 2011 [cited 2019 Dec 20] Available from: https://apps.who.int/iris/bitstream/handle/10665/44697/9799241564359_eng.pdf;jsessionid=3F40A5ABDA6D4164E0BC20101A99B7C4?sequence=1.
Kessler RC. Epidemiology of women and depression. J Affect Dis. 2003;74(1):5-13. doi: http://dx.doi.org/10.1016/s0165-0327(02)00426-3.
Reddy VM, Chandrashekar CR. Prevalence of mental and behavioural disorders in India : a meta-analysis. Indian J Psychiatry. 1998;40(2):149-157.
Lemeshow S, Hosmer DW, Klar J, Lwanga SK. Adequacy of Sample Size in Health Studies. England : John Wiley & Sons. Available from: https://apps.who.int/iris/bitstream/handle/10665/41607/0471925179_eng.pdf?sequence=1&isAllowed=y.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi: http://dx.doi.org/10.1046/j.1525-1497.2001.016009606.x.
Poongothai S, Pradeepa R, Ganesan A, Mohan V. Reliability and validity of a modified PHQ-9 item inventory (PHQ-12) as a screening instrument for assessing depression in Asian Indians (CURES-65). J Assoc Physicians India. 2009;57(2):147-152.
Kochhar PH, Rajadhyaksha SS, Suvarna VR. Translation and validation of brief patient health questionnaire against DSM IV as a tool to diagnose major depressive disorder in Indian patients. J Postgrad Med. 2007;53(2):102-107. doi: http://dx.doi.org/10.4103/0022-3859.32209.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi: http://dx.doi.org/10.1046/j.1525-1497.2001.016009606.x.
Poongothai S, Pradeepa R, Ganesan A, Mohan V. Prevalence of depression in a large urban South Indian population--the Chennai Urban Rural Epidemiology Study (CURES-70). PLoS ONE. 2009;4(9):e7185. doi: http://dx.doi.org/10.1371/journal.pone.0007185.
Urvashi, Girdhar S, Chaudhary A. Socio-demographic co-relates of depression among housewives in rural area of district Ludhiana. Int J Community Med Public Health. 2019;6(5):2147-51. doi: http://dx.doi.org/10.18203/2394-6040.ijcmph20191835.
Mathias K, Goicolea I, Kermode M, Singh L, Shidhaye R, Sebastian MS. Cross-sectional study of depression and help-seeking in Uttarakhand, North India. BMJ Open. 2015;5(11):e008992. doi: http://dx.doi.org/10.1136/bmjopen-2015-008992.
Deswal BS, Pawar A. An epidemiological study of mental disorders at pune, maharashtra. Indian J Community Med. 2012;37(2):116-121. doi: http://dx.doi.org/10.4103/0970-0218.96097.
Obadeji A, Oluwole LO, Dada MU, Ajiboye AS, Kumolalo BJ, Solomon OA. Assessment of Depression in a Primary Care Setting in Nigeria using the PHQ 9. J Family Med Prim Care. 2015;4(1):30-4. doi: http://dx.doi.org/10.4103/2249-4863.152246.
Nisar N, Billoo N, Gadit AA. Prevalence of depression and the associated risks factors among adult women in a fishing community. J Pak Med Assoc. 2004;54(10):519-525.
Mumford DB, Saeed K, Ahmad I, Latif S, Mubbashar MH. Stress and psychiatric disorder in rural Punjab. A community survey. Br J Psychiatry 1997;170(5):473-478. doi: http://dx.doi.org/10.1192/bjp.170.5.473.
Husain N, Creed F, Tomenson B. Depression and social stress in Pakistan. Psychol Med. 2000;30(2):395-402. doi: http://dx.doi.org/10.1017/s0033291700001707.
Ali TS, Mogren I, Krantz G. Intimate partner violence and mental health effects: a population-based study among married women in Karachi, Pakistan. Int J Behav Med. 2013;20(1):131-139. doi:10.1007/s12529-011-9201-6.
Chauhan P, Kokiwar PR, Shridevi K, Katkuri S. A study on prevalence and correlates of depression among elderly population of rural South India. Int J Community Med Public Health. 2016;3(1):236-239. doi: http://dx.doi.org/10.18203/2394-6040.ijcmph20151569.
Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D. Risk factors for common mental disorders in women. Population-based longitudinal study. Br J Psychiatry. 2006;189(6):547-555. doi:10.1192/bjp.bp.106.022558.
Luni FK, Ansari B, Jawad A, Dawson A, Baig SM. Prevalence of depression and anxiety in a village in Sindh. J Ayub Med Coll Abbottabad. 2009;21(2):68-72.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


