A Critical Review on the Effect of Particulate Matter (PM) in Air on Public Health
Mukhopadhyay D.1, Swaminathan J.2*, Kumar Sharma A.3, Basu S.4, Patel P.5, Mukherjee D.6
DOI: https://doi.org/10.17511/ijphr.2021.i02.02
1 Debraj Mukhopadhyay, Department of Public Health, School of Allied Health Sciences, Delhi Pharmaceutical Sciences and Research University (DPSRU), New Delhi, India.
2* J. Swaminathan, Assistant Professor, School of Allied Health Sciences, Delhi Pharmaceutical Sciences and Research University (DPSRU), New Delhi, India.
3 Arun Kumar Sharma, Director & Professor, Department of Community Medicine, University College Medical Sciences (UCMS) & Guru Teg Bahadur (G.T.B) Hospital, University of Delhi (D.U), Delhi, India.
4 Soham Basu, Research Scholar, Institute of Forest Ecology, Faculty of Forestry and Wood Technology, Mendel University, Brno, Czech Republic.
5 Parth Patel, H. K. College of Pharmacy, Mumbai, Maharashtra, India.
6 Dattatreya Mukherjee, MBBS Student and Research Assistant, International School, Jinan University, Guangzhou, P.R China.
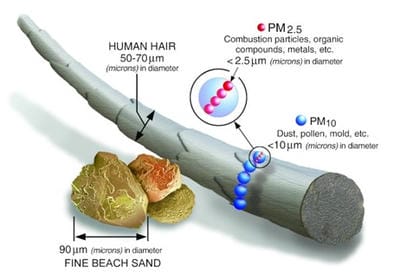
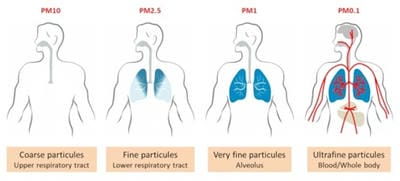
According to the World Health Organization (WHO), particulate matter (PM) contamination causes around 800,000 premature deaths per year, ranking 13th in the world in terms of mortality. However, several findings revealed that the correlation is much stronger and more complicated than previously believed. PM is an element of emissions comprised of very small, acidic, organic compounds, metals, and particulate soil or dust particles or fluid droplets. The most consistent air quality component linked to human illness is PM, which is categorized by size. PM is likely to develop cardiovascular and cerebrovascular disorders due to the mechanisms of inflammation, overt and indirect coagulation activation, and direct translocation to the systemic circulation. The evidence on the cardiovascular system that shows a PM effect is strong. Coronary incidence and mortality rates in populations prone to long-term PM toxicity were significantly higher. Short-term acute emissions increase coronary incidence rates subtly within days of the pollution peak.
Keywords: Air Pollution, Suspended Particulate Matter (SPM), Respiratory Illness, Cardiovascular diseases, Cerebrovascular diseases
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, , School of Allied Health Sciences, Delhi Pharmaceutical Sciences and Research University (DPSRU), , New Delhi, India. Email: |
Mukhopadhyay D, Swaminathan J, Sharma AK, Basu S, Patel P, Mukherjee D. A Critical Review on the Effect of Particulate Matter (PM) in Air on Public Health. Public Health Rev Int J Public Health Res. 2021;8(2):13-22. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/155 |


 ©
©