Secular trends of hospitalization and in-hospital mortality rates of Q-wave and Non-Q-wave myocardial infarction in US: 1990-2006
Nath Ponna S.1*, Rao Pothula N.2, Prasad Upadrasta V.3
DOI: https://doi.org/10.17511/ijphr.2016.i5.04
1* Satyendra Nath Ponna, Scientist-D, Model Rural Health Research Unit, Chittoor, Andhra Pradesh, India.
2 Nageswar Rao Pothula, MD (Internal Medicine), CHRISTUS Spohn Hospital Corpus Christi, Corpus Christi, Texas, United States.
3 Venkata Prasad Upadrasta, Scientist-C, Model Rural Health Research Unit, Chittoor, Andhra Pradesh, India.
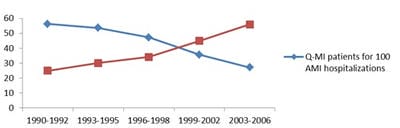
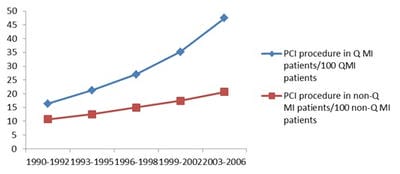
Background: Q-wave and non-Q-wave electrocardiogram (EKG/ECG) findings are proving to be significant prognostic factors for Acute myocardial infarction (AMI) as corroborated from previous studies has implications in patient care. Objective: To document secular changes in proportion of Q-wave myocardial infarction (QWMI) and NQWMI hospitalizations from 1990-2006 and its correlation with changes in demographics and co-morbidities like diabetes mellitus, hypertension and shock, cardiac interventions like PCI and CABG and to investigate change in risk of QWMI and NQWMI death rates from 1990 to 2006. Methods: Trend analysis of QWMI and NQWMI hospitalizations and in-hospital death rates from 1990-2006 of 1,22,841 patients aged ≥35 years admitted for AMI of National Hospital Discharge Survey population-based sample. Trends of QWMI and NQWMI hospitalization and death rates, procedure rates and risk of death from QWMI and NQWMI were documented. Results: The hospitalization rate of QWMI patients decreased from 56 for 100 AMI in 1990 and 92 to 27 for 100 AMI in 2003 and 2006, while hospitalization of NQWMI patients increased from 25 for 100 to 56 for100 AMI. There was increasing trend in PCI procedure rates in both QWMI and NQWMI patients while the trend for CABG procedure rates remained flat in QWMI patients compared to slightly decreasing trends in NQWMI. Conclusions: The increasing trends of NQWMI is in concurrence with increasing trends of diabetes mellitus and hypertension in the population, changes in the diagnostic criteria of AMI and evolution of new treatment patterns of PCI.
Keywords: Acute myocardial infarction, Q-wave Myocardial Infarction, Non-Q-wave Myocardial Infarction, Diabetes Mellitus, PCI, Coronary Artery Bypass Grafting
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Scientist-D, Model Rural Health Research Unit, Chittoor, Andhra Pradesh, India. Email: |
Ponna SN, Pothula NR, Upadrasta VP. Secular trends of hospitalization and in-hospital mortality rates of Q-wave and Non-Q-wave myocardial infarction in US: 1990-2006. Public Health Rev Int J Public Health Res. 2016;3(5):200-209. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/52 |


 ©
©