Knowledge, Attitude and Practices of Parents of Thalassemic Children in District Patiala, Punjab, India
Singh G.1, Mitra Y.2*, Kaur K.3, Bhardwaj K.4
DOI: https://doi.org/10.17511/ijphr.2019.i1.04
1 Gurmeet Singh, Professor, Blood Bank, Government Medical College, Patiala, Punjab, India.
2* Yash Mitra, Assistant Professor, Department of Community Medicine, Punjab Institute of Medical Sciences, Jalandhar, Punjab, India.
3 Kamaldeep Kaur, Medical Officer under DHS, Blood Bank, Government Medical College, Patiala, Punjab, India.
4 Kanchan Bhardwaj, Professor and Head, Blood Bank, Government Medical College, Patiala, Punjab, India.
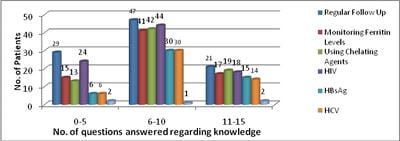
Introduction: β-thalassemia is an autosomal recessive single gene disorder characterized by defective production of hemoglobin and excessive destruction of Red Blood Cells. The defect causes an abnormal development of Red Blood Cells and ultimately anemia. The cultural and religious scenario in Muslims, Khatris and Punjabis migrated from Pakistan is such that consanguineous marriages are quite common. There is no concept of premarital screening of counseling of individuals with a family history of disease. The only way to prevent the disease and to reduce the morbidity and mortality is by educating the general population. Objectives: To assess the Knowledge, Attitude and Practices of Parents of Thalassemic Children. Methods: The study was conducted on parents of 100 patients of thalassemia who are coming regularly for blood transfusion in Thalassemia Day Care Centre (TDCC) run by Patiala Thalassemic Children Welfare Association (PTCWA) at Rajindra Hospital, Patiala to collect the relevant data for the study to evaluate the Knowledge, Attitude and Practices (KAP) of parents of thalassemic children. Results: Mean age of the patients was 8.36 years. 66% patients were males and 34% were females. 41% of the patients were from Khatri community and 59% were from other communities. Family history of thalassemia was present in 23% of the cases and history of consanguineous marriage was present in 4% of the cases. Seventy six percent of the parents knew about the prenatal diagnosis that could be performed to prevent the birth of thalassemic children. Conclusion: There should be a community based educational efforts to increase awareness of this problem especially to the people from low socioeconomic class and from rural area. Control of thalassemia requires treatment of the individual patients as well as a community based educational effort to increase the awareness of this problem.
Keywords: Thalassemic, Glovin, Cultural, Translaplation, Therapy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Community Medicine, Punjab Institute of Medical Sciences, Jalandhar, Punjab, India. Email: |
Singh G, Mitra Y, Kaur K, Bhardwaj K. Knowledge, Attitude and Practices of Parents of Thalassemic Children in District Patiala, Punjab, India. Public Health Rev Int J Public Health Res. 2019;6(1):25-34. Available From https://publichealth.medresearch.in/index.php/ijphr/article/view/97 |


 ©
©