Knowledge, Attitude and Practices of Parents of Thalassemic Children in District Patiala, Punjab, India
Abstract
Introduction: β-thalassemia is an autosomal recessive single gene disorder characterized by defective production of hemoglobin and excessive destruction of Red Blood Cells. The defect causes an abnormal development of Red Blood Cells and ultimately anemia. The cultural and religious scenario in Muslims, Khatris and Punjabis migrated from Pakistan is such that consanguineous marriages are quite common. There is no concept of premarital screening of counseling of individuals with a family history of disease. The only way to prevent the disease and to reduce the morbidity and mortality is by educating the general population. For this reason, present study was taken to evaluate the knowledge, attitude and practices of parents of Thalassemic children.
Objectives: To assess the Knowledge, Attitude and Practices of Parents of Thalassemic Children.
Methods: The study was conducted on parents of 100 patients of thalassemia who are coming regularly for blood transfusion in Thalassemia Day Care Centre (TDCC) run by Patiala Thalassemic Children Welfare Association (PTCWA) at Rajindra Hospital, Patiala to collect the relevant data for the study to evaluate the Knowledge, Attitude and Practices (KAP) of parents of thalassemic children.
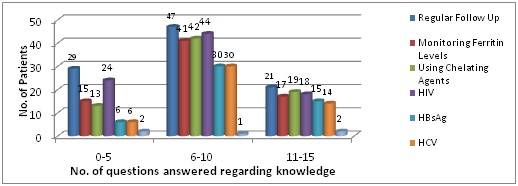
Results: Mean age of the patients was 8.36 years. 66% patients were males and 34% were females. 41% of the patients were from Khatri community and 59% were from other communities. Family history of thalassemia was present in 23% of the cases and history of consanguineous marriage was present in 4% of the cases. Seventy six percent of the parents knew about the prenatal diagnosis that could be performed to prevent the birth of thalassemic children. Knowledge regarding the treatment options available was found more in parents from Bania, Khatri and Kamboj communities. More positive attitude of parents towards prevention of thalassemia was found in parents who have answered 11-15 questions from Knowledge questionnaire.
Conclusion: There should be a community based educational efforts to increase awareness of this problem especially to the people from low socioeconomic class and from rural area. Control of thalassemia requires treatment of the individual patients as well as a community based educational effort to increase the awareness of this problem.
Downloads
References
2. Miglani M, Lokeshwar MR. Transfusion therapy in thalassemia. Manual of Thalassemia 2008; 59.
3. Nair V, Nema SK, Chopra GS, et al. The First Allogeneic Bone Marrow Transplantation in the Armed Forces for Thalassemia. Med J Armed Forces India. 2005 Feb;61(2):190-1. doi: 10.1016/S0377-1237(05)80025-5. Epub 2011 Jul 21.[pubmed]
4. Lokeshwar MR, Shah N, Makrand D, Lokeshwar D, Thalassemia: Approach to the diagnosis. Manual of Thalassemia 2008; 3.
5. Kukreti R, Dash D, E VK, et al. Spectrum of beta-thalassemia mutations and their association with allelic sequence polymorphisms at the beta-globin gene cluster in an Eastern Indian population. Am J Hematol. 2002 Aug;70(4):269-77.[pubmed]
6. Madan N, Sharma S, Sood SK, Colah R, HM Bhatia. Frequency of -thalassemia trait and other hemoglobinopathies in northern and western India. Indian J Hum Genet 2010; 16:16-25.
7. Arif F, Fayyaz J, Hamid A. Awareness among parents of children with thalassemia major. J Pak Med Assoc. 2008 Nov;58(11):621-4.[pubmed]
8. Lee YL, Lin DT, Tsai SF. Et al. Disease knowledge and treatment adherence among patients with thalassemia major and their mothers in Taiwan. J Clin Nurs. 2009 Feb;18(4):529-38. doi: 10.1111/j.1365-2702.2007.02150.x.[pubmed]
9. Bandyopadhyay B, Nandi S, Mitra K, Mandal PK, Mukhopadhyay S, Biswas AB. A Comparative Study on Perceptions and Practices Among Parents Of Thalassemic Children Attending Two Different Institutions. Indian Journal of Community Medicine 2003; 28:3.
10. Shukr et. al. Attitude and knowledge of mothers: Attitude and knowledge of mothers with thalassemia major children. Professional Med J 2011; 18(4): 703-708.
11. Yagnik H. Post counselling follow-up of thalassemia in high risk communities. Indian Pediatr. 1997 Dec;34(12):1115-8.[pubmed]
12. Sen P, Mishra CP, Gupta VM. Dr. P. C. Sen Memorial Award--1994. An epidemiological study of risk factors in preschool children of rural areas of Jaunpur District. Indian J Public Health. 1995 Apr-Jun;39(2):58-63.[pubmed]
13. Ishaq F, Abid H, Kokab F, et al. Awareness among parents of β-thalassemia major patients, regarding prenatal diagnosis and premarital screening. J Coll Physicians Surg Pak. 2012 Apr;22(4):218-21. doi: 04.2012/JCPSP.218221.[pubmed]
14. Upadhyay J and Chatterjee S. Assessment of the knowledge of thalassemia in the thalassemia patients and the treatment received by them. The Internet Journal of Hematology 2009; 5:2.
15. Naseri et al. Status of Yang and Children with thalassemia major in Iran. Iran Thalassemia J 1997; 12: 26-49.
16. Ahmad (2007). Attitude towards Genetic Diagnosis in Pakistan : A Survey of Medical and Lega Communities and Parents of Thalassemia Children 2007; 10:3.[pubmed]
17. Karimi M, Johari S, Cohan N. Attitude toward prenatal diagnosis for beta-thalassemia major and medical abortion in Southern Iran. Hemoglobin. 2010;34(1):49-54. doi: 10.3109/03630260903547690.[pubmed]
18. Shaligram et al. Psychological Problems and Quality of Life in Children with thalassemia. Indian J Pediatr 2007; 74(8): 727-30.
19. Zahed L, Mourad FH, Alameddine R, et al. Effect of oral iron chelation therapy with deferiprone (L1) on the psychosocial status of thalassaemia patients. Haematologia (Budap). 2002;31(4):333-9.
Copyright (c) 2019 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


