Comparative clinical efficacy of propolis mouthrinse in the management patients with chronic generalized gingivitis: a randomized clinical trial
Abstract
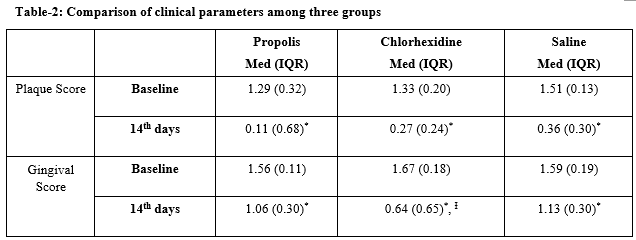
Aim: The aim of the present study was to evaluate the clinical efficacy of propolis and chlorhexidine digluconate containing mouthrinse on a plaque accumulation and gingival inflammation in 14-day period in patients with generalized chronic gingivitis.
Materials & Methods: Thirty subjects were randomly divided into three groups of ten subjects each, which received a propolis-containing mouthrinse, or Saline (a negative control) or Chlorhexidine (a positive control). Plaque and gingival indexes were recorded at baseline and at the end of the 14th days.
Results: Chlorhexidine was the most effective in reducing gingival index compared to the other groups and no significant differences were observed between propolis and saline groups (P<0.05). There were no significant differences among groups for plaque index at the end of the 14th days (P>0.05).
Conclusion: Propolis mouthrinse is promising agent as an alternative to other antimicrobial agents in the mechanical plaque control and gingivitis treatment, but further randomized controlled trials are needed with increased number of individuals.
Clinical Significance: Mechanical plaque control mechanism plays an essential role in reducing microbial burden among patients with gingivitis. However, microorganisms present at many areas of the oral cavity are not mechanically reachable. Therefore, a chemical mechanism; in conjunction with mechanical procedures can play an important role the management of gingival diseases.
Downloads
References
2.LindheJ, KochG.The effect of supervised oral hygiene on the gingiva of children. Lack of prolonged effect of supervision. J Periodont Res. 1967;1(4):215-222. doi: https://doi.org/10.1111/j.1600-0765.1966. tb 01870.x
3.Schou L. Behavioural aspects of dental plague control measures., An oral health promotion perspective. InProceedings of European Workshop on Mechanical Plaque Removal. Berlin 1998 (pp. 287-299). Quintessence, Publishing Co..
4. Renvert S, Glavind L. Individualized instruction and compliance in oral hygiene practices. Recommen-dations and means of delivery. InProceedings of the European Workshop on Mechanical Plaque Removal. pp300-309. Berlin: Quintessence 1998; pp 300-309.
5. Swallow JN, Davies DE, Hawkins SD. Gingival disease prevalence in mentally handicapped adults. The effects of an oral hygiene programme. Br Dent J. 1969;127(8):376-379.
6. Pizzo G, Licata ME, La Cara M, Pizzo I, Guiglia R, Melilli D. The effects of sugar-free chewing gums on dental plaque regrowth: a comparative study. J Dent. 007;35(6):503-508. Epub 2007 Mar 9. doı:10.1016/j. jdent. 2007.01.008
7. Gründemann LJ, Timmerman MF, Ijzerman Y, van der Weijden GA, van der Weijden GA. Stain, plaque and gingivitis reduction by combining chlorhexidine and peroxyborate. J Clin Periodontol. 2000;27(1): 9-15. doı: 10.1034/j. 1600-051x. 2000. 027001009.x
8. Greenstein G, Berman C, Jaffin R. Chlorhexidine. An adjunct to periodontal therapy. J Periodontol. 1986; 57 (6): 370-377. doı:10.1902/jop.1986.57.6.370
9. da Silva WJ, Rached RN, Rosalen PL, Del bel Cury AA. Effects of nystatin, fluconazole and propolis on poly (methyl methacrylate) resin surface. Braz Dent J. 2008; 19(3):190-196. doi:http://dx.doi.org/ 10.1590/ S0103- 64402008000300003
10. Dodwad V, Kukreja BJ. Propolis mouthwash: A new beginning. J Indian Soc Periodontol. 2011; 15(2): 121-125. doi: 10.4103/0972-124X.84379.
11. Molan P. Why honey is effective as a medicine. Part 2. The scientific explanation of its effects. Bee World. 2001;82(1):22-40.
12. Dobrowski JW, Vohora SB, Sharma K, Shah SA, Naqvi SA, Dandiya PC. Antibacterial, antifungal, antiamoebic, antiinflammatory and antipyretic studies on propolis bee products.J Ethnopharmacol. 1991;35 (1): 77–82. doi: https://doi.org/10. 1016/0378-8741(91) 90135-Z
13. Miguel MG, Antunes MD. Is propolis safe as an alternative medicine? J Pharm Bioallied Sci. 2011;3(4): 479-495. doi: 10.4103/0975-7406.90101.
14. Pascual C, Gonzalez R, Torricella RG. Scavenging action of propolis extract against oxygen radicals. J Ethnopharmacol. 1994;41(1-2):9-13. doı:10.1016/0378-8741(94)90052-3
15. Lin SC, Lin YH, Chen CF, Chung CY, Hsu SH. The hepatoprotective and therapeutic effects of propolis ethanol extract on chronic alcohol-induced liver injuries. Am J Chin Med.1997;25(3-4):325-332. doı: 10. 1142/ S0192415X97000366
16. Dobrowolski JW, Vohora SB, Sharma K, Shah SA, Naqvi SA, Dandiya PC. Antibacterial, antifungal, antiamoebic, antiinflammatory and antipyretic studies on propolis bee products.J Ethnopharmacol. 1991; 35 (1) :77-82. doı:10.1016/0378-8741(91)90135-z
17. Khayyal MT, el-Ghazaly MA, el-Khatib AS. Mechanisms involved in the antiinflammatory effect of propolis extract. Drugs Exp Clin Res. 1993; 19 (5):197-203.
18. Mirzoeva OK, Calder PC. The effect of propolis and its components on eicosanoid production during the inflammatory response. Prostaglandins Leukot Essent Fatty Acids. 1996;55(6):441-449.
19. Choi YH, Lee WY, Nam SY, Choi KC, Park YE. Apoptosis induced by propolis in human hepatocellular carcinoma cell line. Int J Mol Med. 1999;4(1):29-32. doı:10.3892/ijmm.4.1.29
20. Marcucci MC. Propolis: chemical composition, biological properties and therapeutic activity. Apidologie. 1995; 26(2): 83-99. doi: https://doi.org/10. 1051 / apido:19950202
21. Wade C, Friedrich JA. Propolis power plus: The health-promoting properties of the amazing beehive energizer. 1st ed. New Canaan, CT: Keats;1996.
22. Koo H, Gomes BP, Rosalen PL, Ambrosano GM, Park YK, Cury JA. In vitro antimicrobial activity of propolis and Arnica montana against oral pathogens. Arch Oral Biol. 2000;45(2):141-148. doı:10.1016/ s0003-9969 (99)00117-x
23. Madarova L. Antibacterial properties of propolis. Ceskoslovenska Stomatologie 1980; 80: 304-307.
24. Scheller S, Ilewicz L, Luciak M, Skrobidurska D, Stojko A, Matuga W. Biological properties and clinical application of propolis. IX. Experimental observation on the influence of ethanol extract of propolis (EEP) on dental pulp regeneration. Arzneimittelforschung. 1978; 28 (2):289-291.
25. Martínez Silveira G, Gou Godoy A, Oña Torriente R, Palmer Ortiz MC, Falcón Cuéllar MA. [Preliminary study of the effects of propolis in the treatment of chronic gingivitis and oral ulceration]. Rev Cubana Estomatol. 1988;25(3):36-44.
26. Santos FA, Bastos EM, Rodrigues PH, de Uzeda M, de Carvalho MA, Farias Lde M, et al. Susceptibility of Prevotella intermedia/ Prevotella nigrescens (and Porphyromonas gingivalis) to propolis (bee glue) and other antimicrobial agents. Anaerobe. 2002;8(1):9-15. doı:10.1006/anae.2002.0411
27. Gómez-Caravaca AM, Gómez-Romero M, Arráez-Román D, Segura-Carretero A, Fernández-Gutiérrez A. Advances in the analysis of phenolic compounds in products derived from bees. J Pharm Biomed Anal. 2006; 41(4): 1220-1234. doi: https://doi.org/10.1016/j. jpba.2006.03.002 Epub 2006 Apr 18.
28. Botushanov PI, Grigorov GI, Aleksandrov GA. A clinical study of a silicate toothpaste with extract frompropolis. Folia Med (Plovdiv).2001; 4 3(1-2):28-30
29. Gebaraa EC, Pustiglioni AN, de Lima LA, Mayer MP. Propolis extract as an adjuvant to periodontal treatment. Oral Health Prev Dent. 2003;1(1):29-35.
30. Charles CA, McGuire JA, Sharma NC, Qaqish J. Comparative efficacy of two daily use mouthrinses: randomized clinical trial using an experimental gingivitis model. Braz Oral Res. 2011; 25 (4): 338-344.
31. Sılness J, Loe H. Perıodontal dısease ın pregnancy. II. Correlatıon between oral hygıene and perıodontal condtıon. Acta Odontol Scand. 1964;22:121-135.
32. Loe H, Sılness J. Perıodontal dısease ın pregnancy. I. Prevalence and severıty. Acta Odontol Scand. 1963; 21:533-551. doi:https://doi.org/10.3109/0001635 63090 11240
33. Beltrami M, Bickel M, Baehni PC. The effect of supragingival plaque control on the composition of the subgingival microflora in human periodontitis. J Clin Periodontol. 1987; 14(3):161-164. doı:10.1111/j.1600-051x. 1987.tb00960.x
34. Bral M, Brownstein CN. Antimicrobial agents in the prevention and treatment of periodontal diseases. Dent Clin North Am. 1988;32(2):217-241.
35. Eley BM. Antibacterial agents in the control of supragingival plaque--a review. Br Dent J. 1999; 186 (6):286-296. doı:10.1038/sj.bdj.4800090
36. Fine DH. Chemical agents to prevent and regulate plaque development. Periodontol 2000. 1995;8(1):87-107. doi: https://doi.org/10.1111/j.1600-0757.1995. tb0 0047.x
37. Herrera D. Chlorhexidine mouthwash reduces plaque and gingivitis. Evid Based Dent. 2013; 14(1): 17-18. doi: 10.1038/sj.ebd.6400915.
38. Van Strydonck DA, Slot DE, Van der Velden U, Van der Weijden F. Effect of a chlorhexidine mouthrinse on plaque, gingival inflammation and staining in gingivitis patients: a systematic review. J Clin Periodontol. 2012;39(11):1042-1055. doi: 10.1111 /j.1600-051X.2012.01883.x. Epub 2012 Sep 7.
39. Ozan F, Sümer Z, Polat ZA, Er K, Ozan U, Deger O.Effect of mouthrinse containing propolis on oral microorganisms and human gingival fibroblasts. Europe J Dent. 2007;1(4):195-201.
40. Dodwad V, Kukreja BJ. Propolis mouthwash: A new beginning. J Indian Soc Periodontol. 2011; 15(2): 121-125. doi: 10.4103/0972-124X.84379.
Copyright (c) 2019 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


