Socio-demographic determinants of Iron and folic acid (IFA) consumption by females during their antenatal period delivering in a tertiary care hospital of Haryana
Abstract
Introduction: In India, the major causes of maternal mortality are hemorrhage (26%) and anemia (19%). According to NFHS -4 data, 53% of women are anemic, this situation further worsens when these anemic women come into the antenatal phase, as there is haemodilution during pregnancy. In Haryana, only 32.5% (NFHS-4, India- 30.3%) mothers had taken 100 IFA tablets during her pregnancy. IFA tablets are being provided free of cost during antenatal visits/checkups but even then its consumption is low whose reasons need to be found out.
Aim and objectives: To find out the socio-demographic factors affecting Iron and Folic acid consumption among recently delivered women.
Material and methods: A cross-sectional study was carried out from April 2017- April 2018 among 500 pregnant females who recently delivered at PGIMS Rohtak. A simple random sampling technique was followed. An interview schedule was used for data collection and data were analyzed using SPSS. A Chi-square test was applied.
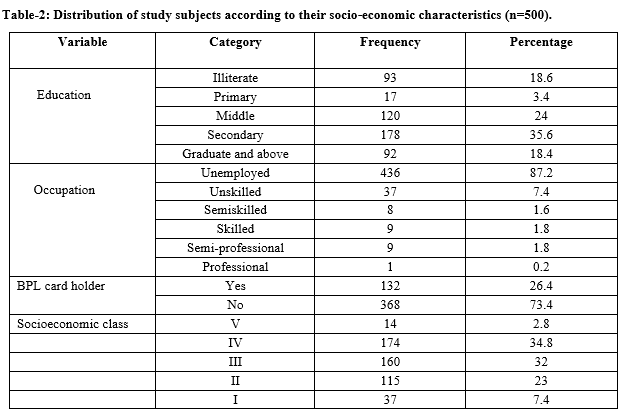
Results: Out of 500 study subjects, the majority (70.4%) belonged to rural area.97.4% of them were Hindus, 81.4% were literate, 77.2% were unemployed, only 26.4% belonged to below poverty line. 80% of subjects were anemic and only 38.2% of study subjects consumed 100 or more IFA tablets. A significant (p≤ 0.05) association was found between IFA consumption and age, education, and occupation. The influence of caste, family type, socio-economic status, and religion was not statistically significant (p>0.05).
Conclusion: Women and their family members need to be educated regarding the consumption of IFA tablets and their role in pregnancy.
Downloads
References
World Health Organization. Maternal mortality, Fact sheet – 19 Sep 2019 [Internet]. Geneva: World Health Organization; 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
Anand T, Rahi M, Sharma P, Ingle GK. Issues in prevention of iron deficiency anemia in India. Nutri. 2014;30(7-8):764-770. doi: https://doi.org/1016/j.nut.2013.11.022.
Government of India. Special bulletin on maternal mortality in India [Internet]. New Delhi: Office of the Registrar General, Government of India; Sample Registration System:2019 [cited 2020 April 23]. Available from: http://censusindia.gov.in/vital_statistics/SRS_Bulletins/MMR_Bulletin-2015-17.pdf
Ministry of Health and Family Welfare. National Family Health Survey-4, India Fact Sheet [Internet]. International Institute of Population Sciences; Government of India; 2015-16 [Cited 2019 Dec 27]. Available from: http://www.rchiips.org/NFHS/pdf/NFHS4/India.pdf. [Last accessed on 2018 Apr 01]
United Nations Children Emergency Fund (UNICEF). State of world’s children report-2014 [Internet]. New York; UNICEF: 2014. Available at: https://www.unicef.org/sowc/
Ahamed F, Yadav K, Kant S, Saxena R, Bairum M, Pandav CS. Effect of directly observed oral iron supplementation during pregnancy on iron status in a rural population in Haryana: A randomized controlled trial. Indian J Public Health.2018;62(4):287-293. Available from: http://www.ijph.in/article.asp?issn=0019-557X;year=2018;volume=62;issue=4;spage=287;epage=293;aulast=Ahamed.
Ministry of Health and Family Welfare. Guidelines for Control of Anaemia: Intensified National Iron Plus Initiative. New Delhi, Government of India; 2018. Available from: https://www.fitterfly.com/site/pdf/anemia-mukt-bharat.pdf
Habib F, Alabdin EH, Alenazy M, Nooh R. Compliance to iron supplementation during pregnancy. J Obstet Gynaecol. 2009;29(6):487-492. doi: https://doi.org/10.1080/01443610902984961.
Lacerte P, Pradipasen M, Temcharoen P, Imamee N, Vorapongsathorn T. Determinants of adherence to Iron/Folate supplementation during pregnancy in two provinces in Cambodia. Asia Pac J Public Health. 2011;23(3):315-323. doi: https://doi.org/10.1177/1010539511403133.
Yip R. Iron supplementation: Country level experiences and lessons learned. J Nutr. 2002;132(4):859S-861S. doi: https://doi.org/10.1093/jn/132.4.859S.
Bora R, Sable C, Wolfson J, Boro K, Rao R. Prevalence of anemia in pregnant women and its effect on neonatal outcomes in Northeast India. J Mat: Fet Neonat Med. 2013;27(9):887-891. doi: https://doi.org/10.3109/14767058.2013.845161.
Mishra S, Gupta P, Bhardwaj P, Sachan B, Srivastav J, Mishra A. effect of antenatal services during pregnancy on prevalence of anemia amongst pregnant women in Lucknow. Indian J Med Sci. 2016;68(1):17. doi: https://doi.org/10.18203/issn.0019-5359.IndianJMedSci20163524.
Ahankari A, Bapat S, Myles P, Fogarty A, Tata L. Factors associated with preterm delivery and low birth weight: a study from rural Maharashtra, India. F1000 Res. 2017;6:72. doi: https://doi.org/10.12688/f1000research.10659.1.
Devineni K, Sodumu N. A study of spectrum of referral pattern at a tertiary teaching hospital towards better obstetric care. IAIM. 2016;3(8):193-198.
Iyengar S, Iyengar K, Gupta V. Maternal Health: A Case Study of Rajasthan. J Health, Population Nutri. 2009;27(2):271-292. doi: https://doi.org/10.3329/jhpn.v27i2.3369.
Malik JS, Kalhan M, Punia A, Sachdeva S, Behera BK. Utilization of Health Services under Janani Suraksha Yojna in Rural Haryana. Int J Med Public Health. 2013;3(3):176-179. doi: https://doi.org/10.4103/2230-8598.118977.
Abdullahi H, Gasim G, Saeed A, Imam A, Adam I. Antenatal iron and folic acid supplementation use by pregnant women in Khartoum, Sudan. BMC Research Notes. 2014;7(1):498. doi: https://doi.org/10.1186/1756-0500-7-498.
Mithra P, Unnikrishan B, Rekha T, Nithin K, Mohan K, Kulkarni V, et al. Compliance with iron-folic acid (IFA) therapy among pregnant women in an urban area of south India. Afr Health Sci. 2013;13(4):880-885. doi: https://doi.org/10.4314/ahs.v13i4.3.
Knudsen VK, Hansen HS, Ovesen L, Mikkelsen TB, Olsen SF. Iron supplement use among Danish pregnant women. Public Health Nutr. 2007;10(10):1104-1110. doi: https://doi.org/10.1017/S136898000769956x.
Wendt A, Stephenson R, Young M, Webb Girard A, Hogue C, Ramakrishnan U, et al. Individual and Facility-Level Determinants of Iron and Folic Acid Receipt and Adequate Consumption among Pregnant Women in Rural Bihar, India. PLoS ONE. 2015;10(3):e0120404. doi: http://dx.doi.org/10.1371/journal. pone.0120404.
Begum S. Factors associated with adherence to iron folic acid supplementations during pregnancy in Uttar Pradesh. Indian J Mater Child Health. 2012;14(2):2-9.
Ankita C, Chandra P, Ashish A. Factors influencing the consumption of iron and folic acid supplementations in high focus states of India. Clin Epidemiol and Glob Health. 2017;5(4):180-184. doi: http://dx.doi.org/10.1016/j.cegh.2017.04.004.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


