Impacts on dietary habits and health of Indian population during COVID-19 lockdown
Abstract
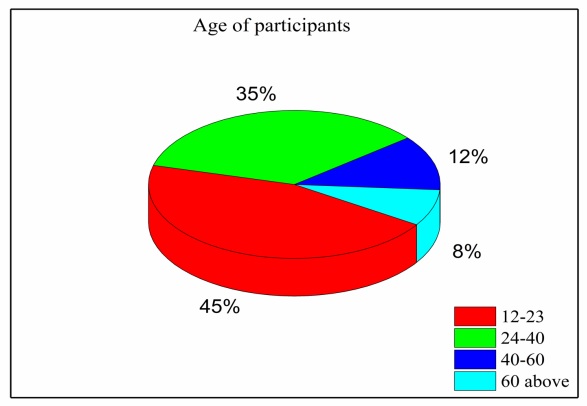
In late 2019 the outbreak of a novel infectious coronavirus (SARS CoV2) which became global pandemic and named as Coronavirus disease (CoViD-19) World Health Organization (WHO). On 22 March, 2020 the Prime Minister of India announced and 14 hours’ public curfew and from 24 March, 2020 announced sudden complete lockdown. The sudden complete lockdown made changes in the living habits and social behaviors of public. Web based survey was conducted among the Indian population of different age groups to understand the impacts on dietary habits and health during the sudden complete lockdown in India.
Downloads
References
Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. The Lancet. 2020;395(10223):470-473. doi: 10.1016/S0140-6736(20)30185-9.
Velavan TP, Meyer CG. The COVID‐19 epidemic. Tropical Med Int ealth. 2020;25(3):278. doi: 10.1111/tmi.13383.
FAQ—Covid-19, domande erisposte. http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioFaqNuovoCoronavirus.jsp?lingua=italiano&id=228#11. Accessed 7 May 2020.
Abenavoli L, Cinaglia P, Luzza F, Gentile I, Boccuto L. Epidemiology of coronavirus disease outbreak: the Italian trends. Rev Recent Clin Trials. 2020;15. https://unigastro.it/Allegati/Epidemiology%20of%20Coronavirus%20Disease%20Outbreak%20The%20Italian%20Trends.pdf
GazzettaUfciale. https://www.gazzettaufficiale.it/eli/id/2020/03/09/20A01558/sg. Accessed 7 May 2020.
Moynihan AB, Van Tilburg WA, Igou ER, Wisman A, Donnelly AE, Mulcaire JB. Eaten up by boredom: Consuming food to escape awareness of the bored self. Frontiers in psychology. 2015;6:369. DOI:https://doi.org/10.3389/fpsyg.2015.00369
Yılmaz C, Gökmen V. Neuroactive compounds in foods: occurrence, mechanism and potential health effects. Food Research International. 2020;128:108744. DOI:https://doi.org/10.1016/j.foodres.2019.108744
Rodríguez-Martín BC, Meule A. Food craving: new contributions on its assessment, moderators, and consequences. Frontiers in PSYCHOLOGY. 2015;6:21. DOI: https://doi.org/10.3389/fpsyg.2015.00021
Ma Y, Ratnasabapathy R, Gardiner J. Carbohydrate Craving-not everything is sweet. Current opinion in clinical nutrition and metabolic care. 2017;20(4):261. DOI: 10.1097/MCO.0000000000000374
Wu C, Chen X, Cai Y, Zhou X, Xu S, Huang H, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA internal medicine. 2020. DOI:10.1001/jamainternmed.2020.0994
Muscogiuri G, Pugliese G, Barrea L, Savastano S, Colao A. Comentary: Obesity: The “Achilles heel” for COVID-19? Metabolism-Clinical and Experimental. 2020;108. DOI:https://doi.org/10.1016/j.metabol.2020.154251
Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. DOI: https://doi.org/10.3390/ijerph17051729
Montemurro N. The emotional impact of COVID-19: From medical staff to common people. Brain, behavior, and immunity. 2020. DOI: 10.1016/j.bbi.2020.03.032
Van Strien T. Causes of emotional eating and matched treatment of obesity. Current diabetes reports. 2018;18(6):35. DOI: https://doi.org/10.1007/s11892-018-1000-x
Evers C, Dingemans A, Junghans AF, Boevé A. Feeling bad or feeling good, does emotion affect your consumption of food? A meta-analysis of the experimental evidence. Neuroscience & Biobehavioral Reviews. 2018;92:195-208. DOI: https://doi.org/10.1016/j.neubiorev.2018.05.028
Singh M. Mood, food, and obesity. Frontiers in psychology. 2014;5:925. DOI: https://doi.org/10.3389/fpsyg.2014.00925
Havermans RC, Vancleef L, Kalamatianos A, Nederkoorn C. Eating and inflicting pain out of boredom. Appetite. 2015;85:52-7. DOI: https://doi.org/10.1016/j.appet.2014.11.007
Crockett AC, Myhre SK, Rokke PD. Boredom proneness and emotion regulation predict emotional eating. Journal of health psychology. 2015;20(5):670-80. DOI: https://doi.org/10.1177/1359105315573439
Muscogiuri G, Barrea L, Annunziata G, Di Somma C, Laudisio D, Colao A, et al. Obesity and sleep disturbance: the chicken or the egg? Critical reviews in food science and nutrition. 2019;59(13):2158-65. DOI: https://doi.org/10.1080/10408398.2018.1506979
Pugliese G, Barrea L, Laudisio D, Salzano C, Aprano S, Colao A, et al. Sleep apnea, obesity, and disturbed glucose homeostasis: epidemiologic evidence, biologic insights, and therapeutic strategies. Current Obesity Reports. 2020;9(1):30-38. doi: 10.1007/s13679-020-00369-y.
Muscogiuri G, Barrea L, Aprano S, Framondi L, Di Matteo R, Laudisio D, et al. Sleep quality in obesity: does adherence to the mediterranean diet matter? Nutrients. 2020;12(5):1364. doi: 10.3390/nu12051364.
Engin AB, Engin ED, Engin A. Two important controversial risk factors in SARS-CoV-2 infection: obesity and smoking. Environmental Toxicology and Pharmacology. 2020:103411. doi: 10.1016/j.etap.2020.103411.
AYUSH T. Ayurveda’s immunity boosting measures for self care during COVID 19 crisis. YaN The Ministry of Ayurvedic, Unani, Siddha and Homeopathy (AYUSH), editor. 2020. Available at www.ayush.gov.in,
Control CfD, Prevention. People who are at higher risk for severe illness Available at https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/peopleat-higher-risk.html. Accessed on April. 2020;1.25.
Dietz W, Santos‐Burgoa C. Obesity and its Implications for COVID‐19 Mortality. Obesity. 2020;28(6):1005. doi: 10.1002/oby.22818.
Zisberg A, Gur-Yaish N, Shochat T. Contribution of routine to sleep quality in community elderly. Sleep. 2010;33(4):509-514. doi: 10.1093/sleep/33.4.509.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


