Socioeconomic inequality of catastrophic health expenditure in Manipur
Abstract
Background: The incidence of catastrophic health expenditure (CHE) is one of the indicators for monitoring the performance of a health system in protecting the financial hardship after availing the service. Further CHE has also raised the issue of equity.
Aim & Objective: To explored the determinants of CHE and also to measure the extent and contribution of socioeconomic factors in CHE in Manipur.
Settings and Design: Manipur is a small hilly state located in the north-eastern region of India. The health expenditure in Manipur as part of the GSDP is very low and stands at 2.79%. This has made rapid growth and expansion of private health care in the state. A cross –section study of primary data of 200 households consisting of 1130 individuals reporting hospitalization during the last 365 days (during 2016) were identified and surveyed.
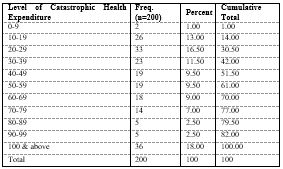
Methods and Material: The incidence of CHE was defined when total health expenditure exceeds 10% of the total household expenditure. The OLS regression has been adopted to identify the significant factors of CHE. Concentration index and decomposition analysis are used to measure the degree of socioeconomic inequality and its contributing factors respectively in Manipur.
Results: The results show that the wealth index, economic crunch (p=0.022), type of disease (Neoplasm (p<0.01) & Genitourinary (p<0.05), the total number of episodes (p<0.05) and duration of stay in hospital (p<0.05) are found to be the significant factors in determining CHE. The concentration index and decomposition analysis indicate that the wealth index plays a vital role in socioeconomic inequality in CHE.
Conclusions: The study reveals that the CHE mainly concentrates among the poor household and intervention of health protection schemes should mainly be focused among the socially as well as economically backward households.
Downloads
References
1. Wagstaff A, Flores G, Smitz MF, Hsu J, Chepynoga K, Eozenou P. ( 2018). Progress on impoverishing health spending in 122 countries: a retrospective observational study. Lancet Glob Heal. 6(2):e180–92.
2. Government of India. Ministry of Health and Family Welfare. (2016). Household Health Expenditures in India (2013-14). 1–44. www.mohfw.gov.in
3. Berki SE. (1986). A look at catastrophic medical expenses and the poor. Health Aff. 5(4):138–45. 4. Wagstaff A, van Doorslaer E. (2001). Paying for Health Care. Quantifying Fairness, Catastrophe, and Impoverishment, with Applications to Vietnam, 1993-98. Policy Res Work Pap 2715.11; 1–50.
5. Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. (2003). Household catastrophic health expenditure: A multicountry analysis. Lancet. 362 (9378):111–7.
6. O’donnell O, Rannan-Eliya RP, Hanvoravongchai P, Huq MN, Karan A, Leung GM, et al. (2005) Explaining the incidence of catastrophic expenditures on health care: Comparative evidence from Asia.
7. Bonu S, Bhushan I, Rani M, Anderson I. (2009). Incidence and correlates of “catastrophic” maternal health care expenditure in India. Health Policy Plan. 24(6):445–56.
8. Vaishnavi SD, Dash U. (2009). Catastrophic payments for health care among households in urban Tamil Nadu, India. J Int Dev. www.wiley.com
9. Lara JLA, Gómez FR. (2011). Determining factors of catastrophic health spending in Bogota, Colombia. Int J Health Care Finance Econ. 11(2):83–100.
10. Waters HR, Anderson GF, Mays J. (2004). Measuring financial protection in health in the United States. Health Policy (New York). 69(3):339–49.
11. Engelgau MM, Karan A, Mahal A.( 2012). The Economic impact of Non-communicable Diseases on households in India. Global Health. 8(1):9. www.globalizationandhealth.com
12. Pandey A, Ploubidis GB, Clarke L, Dandona L. (2018). Trends in catastrophic health expenditure in India: 1993 to 2014. Bull World Health Organ. 96(1):18–28.
13. Devadasan N, Criel B, Van Damme W, Ranson K, Van Der Stuyft P. (2007). Indian community health insurance schemes provide partial protection against catastrophic health expenditure. BMC Health Serv Res. 7:1–11.
14. Li Y, Wu Q, Liu C, Kang Z, Xie X, Yin H, et al. (2014). Catastrophic health expenditure and rural household impoverishment in China: What role does the new cooperative health insurance scheme play? PLoS One. 9(4).
15. Ashour M, Abuzaid A, Korachais C. (2013). Catastrophic health expenditure and entitlement to health services in the occupied Palestinian territory: a retrospective analysis. Lancet. 382:3.
16. Ekman B. (2007). Catastrophic health payments and health insurance: Some counterintuitive evidence from one low-income country. Health Policy (New York). 83(2–3):304–13.
17. Wagstaff A, Lindelow M. (2008). Can insurance increase financial risk? The curious case of health insurance in China. J Health Econ. 27(4):990–1005. www.ncbi.nlm.nih.gov/pubmed.
18. Wagstaff A, Lindelow M, Jun G, Ling X, Juncheng Q. (2009). Extending health insurance to the rural population: An impact evaluation of China’s new cooperative medical scheme. J Health Econ. 28(1):1–19.
19. Shi W, Chongsuvivatwong V, Geater A, Zhang J, Zhang H, Brombal D. (2011). Effect of household and village characteristics on financial catastrophe and impoverishment due to health care spending in Western and Central Rural China : A multilevel analysis. Heal Res Policy Syst. 9(1):16. www.health-policy-systems.com
20. Census MP 2011-2020. Manipur Population Sex Ratio in Manipur Literacy rate data 2011- 2020. www.census2011.co.in/census/state/manipur.
21. Office of The Registrar General of India. (2019). Sample Registration System. Govt. India. 52(1):1–9. www.censusindia.gov.in.
22. CBHI, MHFW G. (2019). National Health Profile (NHP) of India- 2019 : Ministry of Health and Family Welfare. www.cbhidghs.nic.in.
23. William Savedoff. (2003).WHO | How much should countries spend on health? p. 1–14. www.who.int/health_financing/documents
24. International Institute for Population Sciences. ( 2017). National Family Health Survey (NFHS- 4) 2015-16 India. Int Inst Popul Sci ICF. 1–192.
25. Almasian Kia A, Goodarzi S, Asadi H, Khosravi A, Rezapour A. (2019). A decomposition analysis of inequality in malnutrition among under five children in Iran: Findings from multiple indicator demographic and health survey, 2010. Iran J Public Health. 48(4):748–57.
26. Rezaei S, Hajizadeh M. (2019). Measuring and decomposing socioeconomic inequality in catastrophic healthcare expenditures in Iran. J Prev Med Public Health. 52(4):214–23.
27. Kakwani N, Wagstaff A, van Doorslaer E. (1997). Health Inequality. Journal of Econometrics. Vol. 77.
28. van Doorslaer E, Koolman X. (2004). Explaining the differences in income-related health inequalities across European countries. Health Econ. 13(7):609–28.
29. O’Donnell, Owen; van Doorslaer, Eddy; Wagstaff, Adam; Lindelow M. (2007). Analyzing health equity using household survey data : a guide to techniques and their implementation (English) The World Bank. International Bank for Reconstruction and Development. www.worldbank.org.
30. Wagstaff A, Van Doorslaer E, Watanabe N. (2003). On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J Econom. 112(1):207– 23.
31. Choi JW, Kim TH, Jang SISY, Jang SISY, Kim WR, Park EC. (2016). Catastrophic health expenditure according to employment status in South Korea: A population-based panel study. BMJ Open. 6(7):1–7.
32. Kastor A, Mohanty SK. (2018). Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: Do Indian households face distress health financing? PLoS One.13(5):1–18
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


