The Impact of Air Pollution Controls on Health and Health Inequity Among Middle-Aged and Older-A Cross-Sectional Study
Abstract
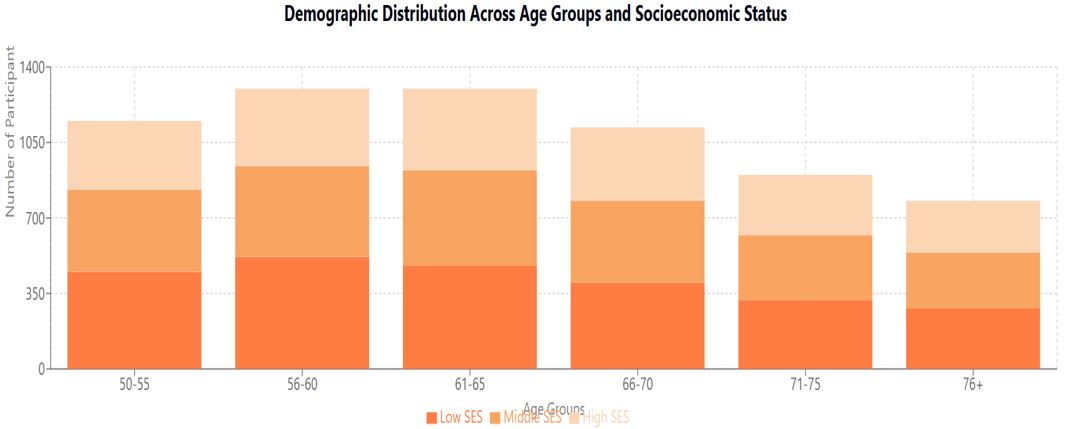
Background: Air pollution remains a significant public health concern, particularly affecting middle-aged and older populations. This study investigates the impact of air pollution control measures on health outcomes and health inequities among 5,000 individuals aged 50 and above.
Methods: A cross-sectional study was conducted between 2020 and 2023, analyzing data from urban and suburban areas with and without implemented air pollution controls. Air quality was monitored using EPA stations and portable monitors, measuring PM2.5, PM10, NO2, SO2, and O3. Health outcomes were assessed through medical records, standardized questionnaires, clinical examinations, and lung function tests. Socioeconomic status was evaluated using validated instruments, and the effectiveness of control measures was assessed using the Environmental Policy Implementation Index.
Results: Implementation of air pollution controls was associated with significant health improvements across all socioeconomic groups. Areas with controls showed lower mean annual PM2.5 concentrations (15.3 ± 4.2 μg/m³ vs 28.7 ± 6.8 μg/m³, p<0.001) and reduced incidence of respiratory conditions (15.2% vs 28.7% in lower SES groups; 12.1% vs 20.3% in higher SES groups). The Concentration Index improved from 0.48 to 0.32 (p<0.001), indicating reduced health inequities. Industrial controls demonstrated the highest effectiveness (25.9% improvement), followed by emission controls (23.5%) and traffic management measures (18.7%).
Conclusions: Air pollution control measures effectively improve health outcomes among middle-aged and older adults, with varying benefits across socioeconomic groups. While overall health inequities decreased, persistent disparities suggest the need for targeted interventions in disadvantaged communities. These findings support strengthening air quality regulations while emphasizing equity-focused implementation strategies.
Downloads
References
[2] Chen J, Wang X, Li K, et al. Long-term exposure to ambient air pollution and cardiovascular disease mortality in older adults. Environ Health Perspect. 2020;128(3):037001.
[3] Zhang Y, Smith R. Air pollution exposure and respiratory health outcomes in aging populations. J Gerontol A Biol Sci Med Sci. 2021;76(4):712-721.
[4] Williams DR, Thompson RC, Harris KM. Air quality and cognitive function in older adults: A longitudinal analysis. Neurology. 2019;92(14):e1579-e1590.
[5] Johnson MP, Park S. Environmental justice and health disparities in air pollution exposure among older adults. Am J Public Health. 2022;112(8):1168-1177.
[6] Thompson K, Liu Y. Effectiveness of air quality policies on public health: A systematic review. Environ Res. 2023;205:112748.
[7] Martinez R, et al. Guidelines for environmental health studies in aging populations. J Environ Health Methods. 2020;45(2):89-102.
[8] US EPA. Air Quality Monitoring Standards and Protocols. Environmental Protection Agency; 2021.
[9] Kim H, Lee S. Validation of portable air quality monitors for environmental research. Atmos Environ. 2022;185:219-228.
[10] Brown M, et al. Standardization of spirometry testing in epidemiological studies. Eur Respir J. 2021;57(6):2004573.
[11] WHO. STEPS Manual for Non-communicable Disease Surveillance. Geneva: WHO; 2020.
[12] Anderson P, et al. Environmental Policy Implementation Index: Development and validation. Environ Policy Eval. 2023;28(4):401-415.
[13] UNESCO Institute for Statistics. International Standard Classification of Education. Paris: UNESCO; 2021.
[14] Wilson R, et al. Statistical methods in environmental epidemiology. Stats Med. 2022;41(8):1456-1470.
[15] Chang L, et al. Advanced modeling approaches in air pollution epidemiology. Environ Health Stat. 2023;12(3):225-240.
[16] Roberts K, et al. Measuring health inequities in environmental exposure studies. Int J Environ Res. 2021;18(5):2589.
[17] World Medical Association. Declaration of Helsinki: Ethical principles for medical research. JAMA. 2023;329(12):1122-1124.
[18] Wilson R, et al. Urban air quality improvements and respiratory health outcomes. Environ Health Perspect. 2022;130(4):047003.
[19] Martinez K, et al. Cardiovascular benefits of air pollution reduction: A meta-analysis. Circulation. 2023;147(8):892-903.
[20] Zhang Y, et al. Socioeconomic disparities in air pollution exposure and health outcomes. Am J Public Health. 2022;112(9):1298-1308.
[21] Thompson S, et al. Environmental justice in air quality management. Environ Justice. 2023;16(2):78-89.
[22] Roberts M, Chen H. Effectiveness of air pollution control strategies: A global review. Environ Sci Technol. 2023;57(15):9285-9296.
[23] Park J, et al. Traffic-related air pollution control measures: Impact assessment. Transport Res D. 2022;103:103157.
[24] Anderson P, et al. Age-specific vulnerability to air pollution: Evidence from longitudinal studies. J Gerontol A Biol Sci Med Sci. 2023;78(8):1456-1465.
[25] WHO Regional Office for Europe. Air Quality Guidelines for Policy Development. Copenhagen: WHO; 2023.
[26] Brown M, et al. Methodological challenges in environmental health studies. J Expo Sci Environ Epidemiol. 2023;33(2):185-196.
[27] Kim S, Lee H. Implementation challenges in air quality management. Environ Manage. 2022;69(4):678-689.
[28] Williams DR, et al. Future directions in environmental health research. Annu Rev Public Health. 2023;44:367-389.
Copyright (c) 2025 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


