A study on the effect of iron folic acid supplementation on the haemoglobin concentration of antenatal cases in field practice area of a rural health centre, Kadapa
Abstract
Introduction: Surveys in different parts of India indicate that about 50 to 60 per cent of women belonging to low socio-economic groups are anemic in the last trimester of pregnancy. The major etiological factors are iron and folic acid deficiencies.
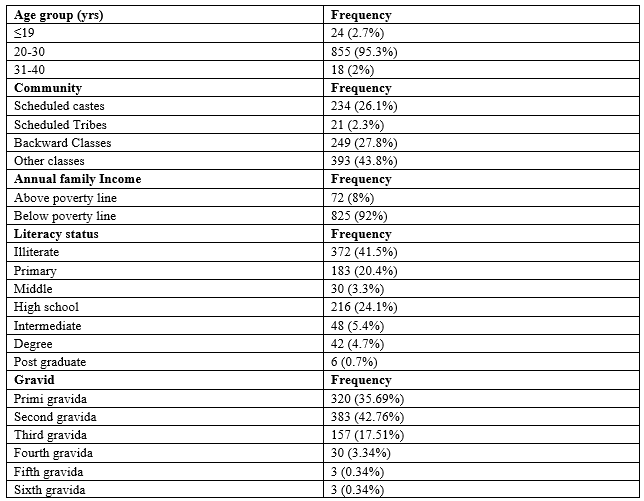
Materials and Methods: In current study baseline data of antenatal cases is recorded with the help of a pre-tested questionnaire. Their blood samples are collected on the date of registration and analyzed for hemoglobin concentration by cyan meth hemoglobin method. First pack of IFA containing 30 tablets is given to the subjects along with administration instructions. These steps were repeated on subsequent antenatal visits at 20, 32 and 36 weeks of pregnancy as per norms. During these subsequent visits hemoglobin concentrations are measured and compliance for IFA supplementation is enquired.
Results: A total of 598 subjects could be followed till the outcome of pregnancy. The mean age was 23.6 yrs. Out of all the risk factors complicating pregnancy most common risk factor was anemia. Most common type of anaemia was due to iron deficiency. Mean Hemoglobin values at the time of registration did not vary significantly in respect to their age groups, community, economic status, gravid status and parity of pregnancy.
Conclusion: Mean Hemoglobin values varied significantly with the literacy status of women. Mean Hemoglobin values varied significantly at every visit with supplementation of IFA. All the women receiving IFA supplementation did not have adequate hemoglobin levels at the time of delivery.
Downloads
References
2. Allen LH. Anaemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr. 2000; 71:1280–4.
3. WHO. Nutritional anaemias: report of a WHO scientific group. Geneva: World Health Organization; 1968
4. DeMayer EM, Tegman A. Prevalence of anaemia in the World. World Health Stat Q. 1998; 38(3):302-16.
5. Gragnolati M, Shekar M, Gupta MD, Bredenkamp C, Lee Y. India’s Undernourished Children: A Call for Reform and Action. Washington, DC: The World Bank; 2005.
6. National Nutrition Monitoring Bureau. Prevalence of Micronutrient Deficiencies. Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 2003.
7. Toteja GS. Micronutrient profile of Indian population. New Delhi: Most India, The USAID Micronutrient Program; 2004.
8. Indian Institute of Population Studies. District Level Household Survey 2 on Reproductive and Child Health: Nutritional status of Children and Prevalence of Anaemia among Children, Adolescents girls and Pregnant Woman. Mumbai: IIPS; 2006.
9. Ramachandran P. Maternal nutrition - effect on foetal growth and outcome of pregnancy. Nutr Rev. 2002 May; 60(suppl 5):26-34.
10. Sifakis S, Pharmakides G, Anaemia in Pregnancy. Ann N Y Acad Sci. 2000 April; 900:125-36.
11. World Health Organization. Iron deficiency anaemia: assessment, prevention and control. A guide for programme managers. Geneva: World Health Organization; 2001. p. 114.
12. Yip R, Ramakrishnan U. Experiences and challenges in developing countries. J Nutr. 2002; 132:827–30.
13. Fairbanks VF. Iron in medicine and nutrition. In: Shils ME, Olson JA, Shike M, editors. Modern nutrition in health and disease, 8th ed. Philadelphia, PA: Lea & Febinger; 1994. p. 185–213.
14. Yip R, Dallman PR. Iron. In: Ziegler EE, Filer LJ Jr, editors. Present knowledge of nutrition, 7th ed. Washington, DC: International Life Sciences Institute Press; 1996. p. 277–92.
15. Allen L, Casterline-Sabel J. Prevalence and causes of nutritional anaemias. In: Ramakrishnan U, editor. Nutritional anaemias. Boca Raton, FL: CRC Press; 2001. p. 7–21.
16. Ethiopia. Federal Ministry of Health. National guideline for control and prevention of micronutrient deficiencies. Addis Ababa: Family Health Department, Federal Ministry of Health, Government of Ethiopia; 2004. p. 26.
17. Stoltzfus R, Dreyfuss M. Guidelines for the use of iron supplements to prevent and treat iron deficiency anaemia. Washington, D. C: International Nutritional Anaemia Consultative Group. ILSI Press; 1998.
18. Institute of Medicine. Iron deficiency anaemia: guidelines for prevention, detection and management among U.S. children and women of childbearing age. Washington, D. C: National Academy Press; 1993.
19. Centre for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. Atlanta: MMWR Recomm Rep. 1998; 47(RR-3):1-29.
20. Micronutrient Initiative. Vitamin and mineral deficiency: a global progress report. Ottawa: Micronutrient Initiative; 2004. p. 39.
21. DeMaeyer EM. Preventing and controlling iron deficiency anaemia through primary health care: a guide for health administrator and programme managers. Geneva: World Health Organization; 1989. p. 58.
22. World Health Organization. Major issues for nutrition strategies of Food and Agriculture Organization and WHO. FAO/WHO International Conference on Nutrition. Geneva: World Health Organization; 1992. p. 12–23.
23. Mishra P, Ahluwalia SK, Garg PK, Kar R, Panda GK, Mishra et al., The Prevalence of Anaemia among Reproductive Age Group (15-45 Yrs) Women in A PHC of Rural Field Practice Area of MM Medical College, Ambala. India J Women’s Health Care. 2012; 1:3.
24. Mondal B, Maiti S, Maiti B, Ghosh D, Paul S. Prevalence of anaemia in pregnant bauri women of bankura, west Bengal, India. Journal of Clinical and Diagnostic Research. 2012 April; 6(2): 231-3.
25. Pandey A, Sengupta B. Socio-Demographic Profile of an Urban Slum of Kolkata, 2013: A Snapshot. Indian Journal of Hygiene and Public Health. 2015 June; 1(1):68 – 75.
26. Ahmad N, Kalakoti P, Bano R, Aarif SMM. The prevalence of anaemia and associated factors in pregnant women in a rural Indian community. Australas Med J. 2010; 3(5):276-80.
27. Shah AR, Patel ND, Shah MH. Haematological parameters in anaemic pregnant women attending the antenatal clinic of rural teaching hospital. Innovative Journal of Medical and Health Science. 2012 Sep-Oct; 2(5):70-3.
28. Goswami TM, Patel VN, Pandya NH, Mevada MK, Desai K, Solanki KB. Maternal anaemia during pregnancy and its impact on perinatal outcome. International Journal of Biomedical and Advance Research. 2014; 5(2):99-102
29. Stevens G, Finucane M, De-Regil L, Paciorek C, Flaxman S, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013 Jul; 1(1):e16-25.
30. World Health Organization. The prevalence of anaemia in women: a tabulation of available information. 2nd ed. Geneva: Maternal Health and Safe Motherhood Programme, Division of Family Health; 1992.
31. Puolakka J, Janne O, Pakarinen A, Vihko R. Serum ferritin as a measure of stores during and after normal pregnancy with and without iron supplements. Acta Obstet Gynecol Scand. 1980; 95(suppl):43–51.
32. Uche-Nwachi EO, Odekunle A, Jacinto S, Burnett M, Clapperton M, David Y, et al., Anaemia in pregnancy: associations with parity, abortions and child spacing in primary healthcare clinic attendees in Trinidad and Tobago. African Health Sciences. 2010 March; 10(1):66-70.
33. Peña-Rosas JP, De-Regil LM, Dowswell T, Viteri TE. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015 Jul; 22(7):CD004736.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


